Back Pain: How Osteopathy Can Help
Back pain is one of the most common reasons people seek osteopathic care. Whether your discomfort is a dull ache or a chronic lower‑back issue, an osteopath will assess how your joints, muscles and posture are working together. Through gentle manipulations, soft‑tissue massage and tailored exercises, osteopathy aims to reduce tension, improve movement and support the body’s healing processes. You’ll also receive advice on posture and core strengthening to help prevent the pain returning.
Understanding Sciatica: Symptoms, Relief and Osteopathy
Sciatica is a term used to describe pain that radiates along the sciatic nerve—the longest nerve in your body, running from the lower back down through the hips, buttocks and legs. It’s not a condition itself, but rather a symptom of something irritating or compressing the nerve. Many people experience sciatic discomfort at some point in their lives, often finding it frustrating and limiting.
What is Sciatica?
Sciatica refers to a set of symptoms rather than a single diagnosis. It usually occurs when part of your lower spine or surrounding tissues put pressure on the sciatic nerve. This can happen for various reasons, such as spinal discs bulging or degenerating, wear and tear in the joints, or temporary swelling around muscles and ligaments.
Common Symptoms of Sciatica
People with sciatica often describe a range of sensations. You may experience some or all of the following:
- Pain radiating from the lower back to the buttock, thigh or even the foot – this pain can be sharp, burning or aching.
- Numbness or tingling in the leg or foot.
- Weakness in the muscles of the leg or foot.
- Pain that worsens when sitting or standing for long periods, or when sneezing or coughing.
- Difficulty moving or controlling the leg or foot, in more severe cases.
These symptoms can vary from person to person and from day to day. Sometimes the pain is only mild and goes away on its own; other times it can be intense and persistent.
What Causes Sciatica?
Sciatica can arise from a number of conditions, including:
- Herniated or slipped discs – when the soft centre of a spinal disc pushes out and irritates the nerve.
- Spinal stenosis – narrowing of the spaces within your spine, which can compress nerves.
- Degenerative disc disease – wear and tear on the discs between the vertebrae.
- Piriformis syndrome – a tight piriformis muscle (deep in the buttock) can irritate the nerve.
- Pregnancy – changes in posture and added weight can put extra strain on the spine.
- Poor posture or prolonged sitting – especially in jobs that require long hours at a desk or behind the wheel.
Understanding what might be causing your sciatica helps guide you toward the right support and management strategy.
When to Seek Osteopathic Support
While many people experience mild sciatica that improves with rest and gentle movement, it’s important to seek professional advice if:
- Your pain lasts more than a couple of weeks or keeps returning.
- The pain is severe enough to interfere with daily activities like walking, sleeping or working.
- You notice increasing numbness, weakness or difficulty controlling your leg or foot.
- You experience bladder or bowel changes – this can be a sign of a more serious condition requiring urgent medical attention.
Speaking with an osteopath can be a helpful first step for non‑emergency cases. They can assess your symptoms, look for underlying issues and help you decide on a care plan.
Self‑Care Tips for Sciatica Relief
There are several things you can do at home to ease discomfort and support your recovery:
- Keep moving gently – long periods of bed rest can make things worse. Gentle walks or stretching can promote circulation and reduce stiffness.
- Apply heat or cold – a warm compress can relax tight muscles, while a cold pack can reduce inflammation. Try both and see which feels better for you.
- Mind your posture – whether you’re sitting at a desk or standing in a queue, aim to keep your spine aligned and avoid slouching.
- Avoid prolonged sitting – get up regularly, stretch or walk around. Consider a standing desk for part of your day.
- Try low‑impact exercise – gentle swimming, yoga or Pilates can strengthen supporting muscles without putting too much strain on the back.
Listen to your body and stop any activity that increases your pain.
How Osteopathy May Help
Osteopathy is a hands‑on approach that focuses on the musculoskeletal system – your muscles, joints and connective tissues. An osteopath will use gentle manual techniques to:
- Release tension in muscles and connective tissues, helping to reduce pressure on the sciatic nerve.
- Improve joint mobility in the spine and pelvis, allowing your body to move more freely.
- Support healthier posture and movement patterns, reducing the likelihood of irritation returning.
While osteopathy does not claim to cure sciatica, many patients find it helps ease discomfort and supports their body’s own recovery processes.
What to Expect at Your Appointment
During your visit, your osteopath will:
- Take a detailed history – learning about your symptoms, lifestyle and medical background.
- Perform a physical assessment – checking your posture, range of motion and areas of tension.
- Provide hands‑on treatment – using gentle techniques tailored to your needs.
- Offer advice – suggesting exercises, stretches or lifestyle adjustments to support your recovery.
Appointments typically last around 30‑45 minutes, and you’ll remain clothed (though you may be asked to remove shoes or outer layers). Treatment should never be painful; always let your practitioner know if you feel discomfort.
Local Support in Kettering & Corby
At Taylor Osteopathy, we see many patients from Kettering, Corby and the wider Northamptonshire area who are dealing with sciatic symptoms. We understand how disruptive nerve pain can be, and we’re committed to providing a friendly, professional space where you can explore your options for relief. If you’re struggling with sciatica, we’re here to discuss how osteopathy may be able to support you.
Final Thoughts
Sciatica can be a painful and sometimes worrying experience, but with the right information and support it is often manageable. By understanding the causes and signs of sciatica, taking steps to look after your posture and movement, and seeking professional advice when needed, you can take back control of your comfort. If you’re in Kettering or Corby and want to know more about osteopathic care for sciatica, our clinic is just a call or click away.
Gardening Without Back Pain – An Osteopath’s Advice
Gardening is a wonderful way to connect with nature, enjoy fresh air and transform your outdoor space. But for many people, long hours spent digging, weeding and carrying heavy pots can leave them with an aching back. If you love tending your garden but hate the stiffness afterwards, this guide will help you stay comfortable and enjoy every season without pain.
Why Gardening Can Hurt Your Back
It’s easy to underestimate just how much bending, twisting and lifting is involved in even simple gardening tasks. Here are a few reasons gardeners often experience back pain:
- Repetitive bending and stooping – planting and weeding require you to lean forward for extended periods, placing strain on the muscles supporting your spine.
- Heavy lifting – bags of soil, watering cans and large pots can be surprisingly heavy, especially if you lift them with your back instead of your legs.
- Twisting motions – reaching for tools or turning quickly while carrying items can cause small muscle strains.
- Awkward postures – working on the ground or in raised beds sometimes encourages you to crouch or overreach, which can irritate joints and soft tissues.
Tips for Gardening Pain-Free
The good news is there are plenty of ways to look after your back while still enjoying time outdoors. Try these simple tips:
- Warm up first
- Do a few gentle stretches before heading outside, focusing on your back, hips and shoulders. This gets your blood flowing and muscles ready for activity.
- Lift with your legs
- When picking up heavy items, bend your knees, keep your back straight and hold the object close to your body. If something feels too heavy, divide the load or ask for help.
- Use ergonomic tools
- Long-handled tools, kneeling pads and wheelbarrows reduce the need to bend and help you maintain good posture. Consider investing in lightweight equipment designed for comfort.
- Mix up your tasks
- Alternate between jobs that use different muscle groups. For example, spend 20 minutes planting, then switch to pruning or watering, rather than bending for an hour straight.
- Take regular breaks
- Stand up, stretch and walk around every 30 minutes to avoid stiffness. Short breaks give muscles a chance to rest and prevent strain from building up.
- Adjust your workspace
- Raise flower beds or use container gardens to minimise bending. A potting bench at waist height can make planting and transplanting much easier on your back.
Local Gardening in Kettering & Corby
Gardening is particularly popular here in Kettering and Corby. Local allotments, community gardens and home plots provide wonderful spaces for residents to grow vegetables, flowers and herbs. If you live in the area, keep in mind that the heavy clay soil common in Northamptonshire can be tricky to work with. Use mulch and compost to improve soil structure and consider raised beds or containers for easier maintenance.
When the weather turns cold or rainy, be mindful of slippery surfaces. Wear sturdy footwear and be extra careful when carrying tools or bags. Staying safe ensures you can enjoy your garden all year round.
How Osteopathy May Help Gardeners
Osteopaths work with the musculoskeletal system – the muscles, joints and tissues that support your body. If you’re experiencing persistent stiffness after gardening, osteopathy may help by:
- Using gentle hands-on techniques to ease muscle tension and improve joint mobility.
- Advising on posture and movement patterns to reduce strain while gardening.
- Suggesting targeted stretches and strengthening exercises tailored to your body and lifestyle.
Many people find that regular osteopathic care helps them stay active and comfortable while pursuing hobbies like gardening. Though osteopathy doesn’t claim to “cure” back pain, it may support your body’s natural ability to recover and move with ease.
When to Seek Advice
A little soreness after a weekend in the garden is normal, but persistent or severe back pain shouldn’t be ignored. If you experience any of the following, consider speaking to an osteopath or healthcare professional:
- Pain that doesn’t improve with rest or gentle stretching.
- Numbness, tingling or weakness in your legs.
- Pain that radiates from your back to your hip or down your leg.
Get Support from Taylor Osteopathy
At Taylor Osteopathy, we love helping local gardeners in Kettering and Corby stay active and pain-free. If gardening is causing you discomfort, get in touch to see how osteopathy may help. We’ll listen to your concerns, assess your movement and offer gentle treatment and advice to get you back in the garden with confidence.
Book an appointment today or call our friendly clinic for more information. Happy gardening!
Inflammation. A tasty rehab soup?
Ice or heat therapy for pain, which should you use? I explain it like this…It’s a soup!

For this recipe you will need:
One piece of soft tissue (muscle, tendon, ligament)
1tsp – Prostaglandin D2
1tsp – prostaglandin E2
½ tsp- prostaglandin F2
½ tsp – prostaglandin I2 (which is also known as prostacyclin)
1tbsp – thromboxane
5ml – Bradykinin
Pinch of histamine to flavour
Method:
- Place the soft tissue in a vulnerable or weakened position. Repeatedly perform a strenuous activity until there is some discomfort. If you prefer to have the tissue already prepared, it may be called injured.
- Mix the remaining ingredients together in a bowl to create inflammation.
- Place the soft tissue on a surface and insert some of the inflammation into the tissue and rub the remainder over the surface.
- Leave to rest overnight, or until you feel; an ache, throbbing, warmth or redness to the tissue, sharp pain when moving.
The result, a delicious inflammatory soup!
Do I treat my injury with ice or heat then?
This is how I explain inflammation to my patients. It begins to make sense when it is broken down into smaller parts. Inflammation is not just one substance.

It is a mixture of many hormones (hormones are chemical messengers that travel through the bloodstream to create a change elsewhere).
In an acute injury the cells surrounding the injured body part release inflammation. The role of each inflammatory hormone is slightly different, but they all in the aid of helping the injured tissue to heal faster.
Some inflammatory hormones interact with blood vessel walls to relax them (vasodilation). This allows more blood flow to the injured tissue which brings with it the healing properties it needs to recover. Other hormones interact with the nerve endings, sending signals to the brain, effectively telling you stop doing what you are doing, or you will damage yourself further. This is a good thing. This signal is called pain.
The idea behind applying heat to an injury is that it vascularises the area. It promotes blood flow to the injured tissue. Helping spasmed or tight muscles to relax, or injured tissue to heal, faster.
This is not to say that only heat should be used. Sometimes injuries are just too painful to deal with.
Discomfort can make it difficult to concentrate on tasks and can also make you partially or completely immobile. Here, ice can help. In this instance, the cold can reduce the inflammation being produced so there is less pain. The outcome of this is that you may be able to concentrate on a task or move more freely which has the effect of relaxing muscles and improving blood flow… But only if you move! Be warned though, this will also increase your healing time, so there is a trade of sorts to be had.
Of course, all of the above assumes the individual has no underlying health concerns such as chronic inflammation or any inflammatory disease.
COVID-19 Facemasks, don’t judge me…
Osteopath, Kettering, COVID-19
Let us rehab safely, welcoming everyone

Your osteopath treatment for neck and back pain hasn’t changed but it seems like since mid-March 2020 everything else has!
The advent of daily lifestyle restrictions, along with forced hygiene and cleanliness protocols in businesses, was necessary to slow the spread of the COVID-19 virus. Thankfully, it worked.
Fast forward 18 months; the schools have reopened, and people are beginning to return to work. Thankfully, life is seemingly getting back to normal.
Looking out my clinic window, I can see people gathering in groups, hugging, and possibly forgetting, or ‘choosing’ to forget, the trials for the last two years. Nationwide restrictions and rules have been relaxed. Fewer people seem to be sanitizing their hands when entering and exiting shops, whilst many are also choosing to not wear masks. To be clear, I pass no judgement on people that decide they do not want to wear face coverings. The rules have relaxed, and those people have decided that they want to try to continue with life as they were pre-March 2020, and that is totally ok.
But…
As primary healthcare professionals, osteopaths, like other allied health professionals, are governed by a body that regulates us as clinicians. The guidelines that are set out to us are to make sure that we can make sure that everybody remains safe. That is what the guidelines are for. As a result of this, all healthcare clinics must advise that patients wear face coverings when arriving for treatment, to reduce the risk of transmission to those that are more vulnerable in our communities.
If a person is medically unable to wear a face-covering or chooses to not wear one due to their personal belief or opinion, we are still able to provide treatment, but the clinic must adjust for your visit. For this reason, many clinics, including our own, will ask that you make yourself available to be either the first or last client of the day. This is so that the clinic rooms can adequately aerate before the next person is due to attend.
It can be a bit of a pain for all involved, but the guidelines are there to help contain the spread of the virus and keep us all safe.
If you have any questions, regarding arranging a consultation, please do not hesitate to contact us. We shall be happy to answer any questions you may have.
Joint pain
Arthritis, joint pain, wear and tear

Pain in one or more joints could be arthritis. In fact, it is. The word ‘arthritis’ derives from the Greek word -artho, meaning ‘joint’, and ‘itis’ meaning inflammation.
Joint pain, stiffness, tenderness, joint inflammation, reduced movement, redness and warmth around the joint, muscular weakness and wasting, can all be symptoms of the disease.
To be honest, arthritis is pretty rubbish. It can restrict a person’s ability to lead an ordinary life. In the clinic, we hear stories of arthritic hips causing pain and an inability to walk for even short distances. Arthritis of the hands making it impossible to open a can of pickled onions and similarly, arthritis in the knees making climbing stairs painful or kneeling on the floor to play with the grandchildren very difficult indeed.
There are four types of arthritis:
- Degenerative arthritis – Of this group, osteoarthritis is the most common. The cartilage that cushions the joint wears done and the joint begins to rub bone against bone, causing discomfort, stiffness and sometimes swelling. The pain persists and the muscles lose strength. Increased weight, previous trauma (ie meniscus tear), age and family history can all be risk factors.
- Inflammatory arthritis – Rheumatoid arthritis, psoriatic arthritis, gout and ankylosing arthritis, are all examples of this disease. Our body is great at keeping us healthy with an immune system. It creates inflammation to rid us of infection and disease, but in some people, this immune system does not work properly. It can be destructive with too much inflammation, causing joint erosion. Scientists believe a person’s environment and genetics may trigger this autoimmune reaction.
- Infectious arthritis – Organisms can sometimes infect our joints causing infectious arthritis. A virus, bacteria or fungus may cause inflammation when entering a joint. Blood infections such as Hepatitis C can cause arthritis. Some sexually transmitted diseases and food poisoning may also cause joint inflammation and pain.
- Metabolic arthritis – Purine, a substance found in many foods and also in human cells is broken down by the body, forming uric acid. In some people, the body produces too much naturally or is unable to rid itself of it quickly enough. When this happens, the build-up of uric acid begins to form sharp, needle-like crystals in joints, which can cause incredible pain for those affected (Gout). If the levels of uric acid are not reduced then the ongoing issue can become chronic, causing temporary pain or ongoing disability.
What you can do
Getting an accurate diagnosis of your condition is the first step. Pain relief medications may help or other medicines may be prescribed depending on the arthritis type. Maintaining movement is essential to keep muscles strong and the joints flexible. Maintaining a healthy weight and improving diet can also help with some types of arthritis. Seeking help and assistance from a qualified osteopath for specific arthritis rehabilitation is also advised, to help reduce the pain felt from this debilitating group of conditions.
The Rotator Cuff
Rotator Cuff tears, impingements and bursitis
Do you have shoulder pain and not know why? It could be your cuff! Rotator cuff injuries a real pain to have to live with. Being unable to freely put on a jumper, carry a shopping bag, lie on your side, or even brush your teeth, can really take the shine out of the day. In fact, most people in the clinic tell us that it’s the simple activities that they usually take for granted that bother them the most. Playing with the children is no longer fun and throwing a ball for the dog is now just not possible.
We are often told, in the clinic, that the attitude of “it will get better by itself soon” leads to months down the line, somehow making things worse. Neck and upper back pain soon follows as the body tries to adapt to a new pattern of movements to help patients avoid the pain of moving the arm. Shoulder pain becomes a real nuisance and the people around you appear to start to suffer because of the patient’s pain too.
After reading the above, if this is you, then a little bit of knowledge of the shoulder and rotator cuff can go a long way here. Understanding some basic biomechanics and the actions of the rotator cuff muscles can help you to understand what may be going on and how to help yourself…So here it is.
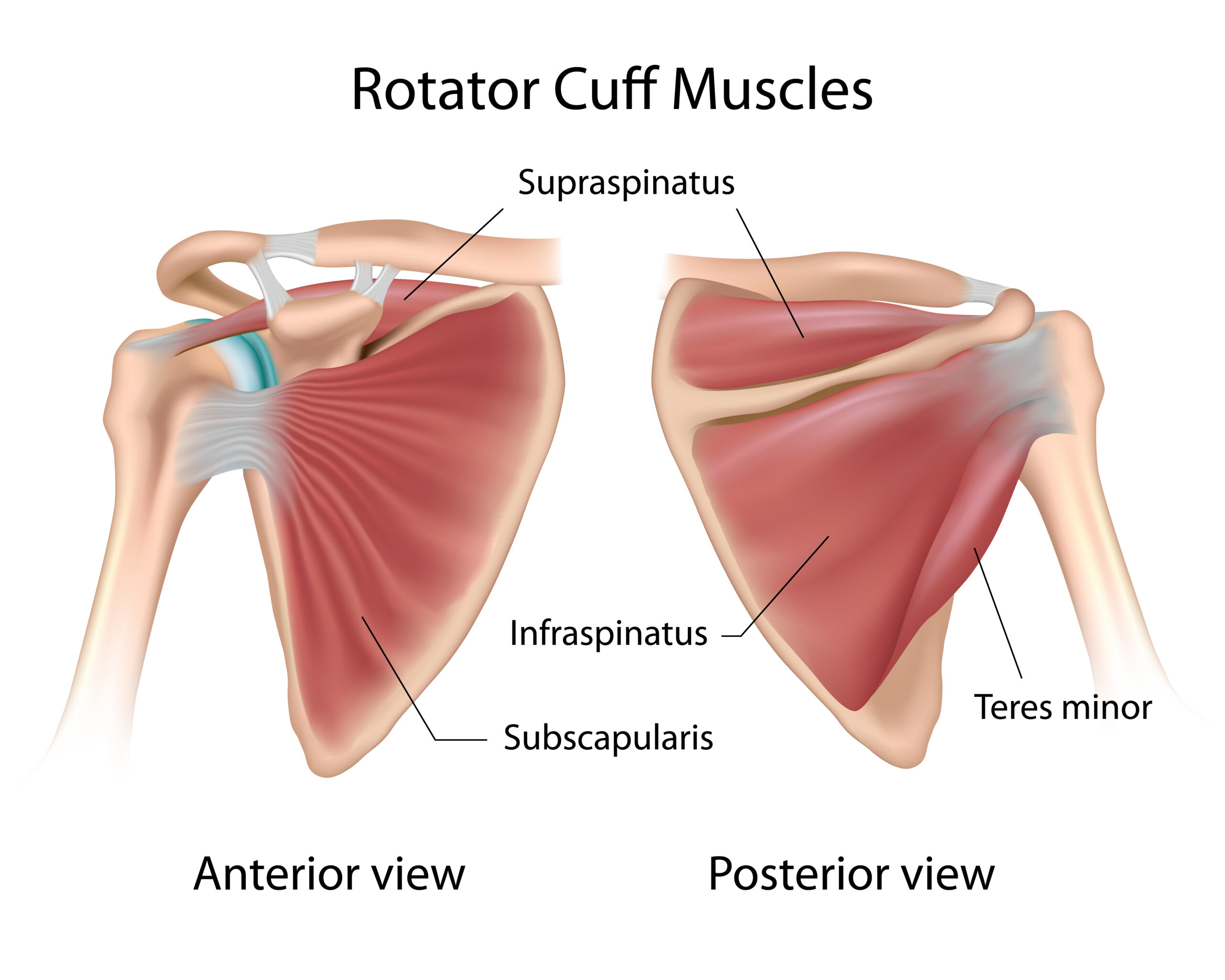
The rotator cuff is made up of four muscles: Supraspinatus, Infraspinatus, Teres Minor and Subscapularis. Now, these names may sound complicated but the jobs these muscles perform are far from it. Their roles may be simple but they are also very VERY important. The rotator cuffs primary role is to hold onto your arm (humerus) and suck it into your shoulder (glenoid fossa). The shoulder is a very mobile joint and due to this, lacks stability. These muscles, therefore, have to work really very hard, especially if you use your arms all day, every day and in repeated motions. These motions after a period of time can start to cause friction between two structures, where the muscle starts to rub against another tissue, for example, a bursa (causing bursitis) or causing micro-trauma to tendons causing micro-tears (tendinitis). These common shoulder issues, bursitis and tendinitis, increase the inflammation around the injured site, which therefore irritates the nerve endings causing you the pain and discomfort you feel.
Shoulder pain, exercises, stretches and rehab
Thankfully there are things that can be done to alleviate some of the discomforts of shoulder impingement, bursitis or tendinitis. Exercise and strengthening the muscles under the guidance of a qualified therapist Will most likely improve your symptoms over time but you can also improve your own symptoms by performing some simple exercises. Personally, I like to advise a simple traction exercise to start. I have attached a link here to a YouTube video that may be of benefit if you are suffering from shoulder pain. Click the link below to take a look:
Back pain, not in the back?
Back pain, not in the back?
A new patient, requesting treatment for a sudden onset of back pain was booked into the Corby clinic yesterday evening. When questioned, requesting the description of the lower back pain it seemed simple enough to understand; sharp and burning pain to the left lower back. This is quite a common description of a trapped nerve and also quite easy to treat too.
When I asked what caused this sudden onset of pain the patient was less sure than her description of her pain. “Nothing happened. The pain just came on”.
Not so simple after all…. Pain does not just happen. There is always a cause. A trip and fall to sprain an ankle, or some arthritis causing pain in the hip or knee. Pain does not arise from just nowhere.
I grew more inquisitive when the patient could not tell me what increased or relieved her pain. So I delved further with my questions. Do you feel sick or bloated? Are you constipated? Do you pain anywhere else? Etc. When the answers to these questions returned no further information, I then turned to the physical examination.
As an osteopath, in an examination, we request that the patient performs set movements to see if we can replicate the pain. If we can then that is fantastic, we have more information to work with. If not, then that too, is still positive, as negative results can help to make some issues more or less likely.
When I was unable to replicate the discomfort in the patients lower back, I was about to request that we perform some orthopaedic tests, when, out of the blue a sharp and burning pain gripped the patient and then passed, just a quickly as it appeared. When I questioned the patient about the pain that just occurred, I found out that the pain was not in the lower back at all but in the thorax, at the bottom of the ribs. This started to ring alarm bells, as the thorax is the area where the major organs, apart from the brain, are positioned.
I performed a few orthopaedic tests and was still unable to replicate the pain that the patient had just experienced, so I decided to perform an abdominal examination, much like the doctor would, if presented with the same case.
I could feel nothing untoward within the abdomen and the patient reported that the examination had caused her no pain and I could not find anything that felt unusual. I had a general idea of what I thought it might be, a kidney infection or stones, neither of which a physical therapist is able to treat, so I had no choice but to refer her back to her GP for further consultation.
I called the patient the next day to find out how she was, and discovered that the GP felt much the same as I did. He had the patient perform a urine test which found traces of infection and blood in her sample too, which could indicate stones. The patient was given antibiotics and pain killers, whilst she is referred to a consultant for more tests.


Recent Comments